To help you understand what happens in the immediate aftermath of a brain injury, we must first explain what traumatic brain injury (TBI) is and how it happens.
Put in the simplest terms, TBI is a term used to describe the harm done to brain tissue or loss of brain tissue caused by a blow to the head incurred from an assault, a car crash, a gunshot wound, a fall, or similar incident. TBI can occur with both open and closed head injuries.
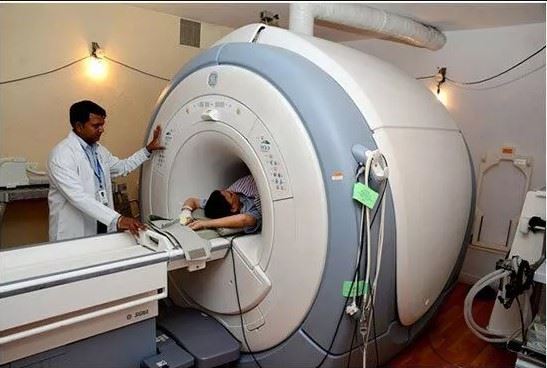
In a closed head injury, a forceful blow to the head causes damage by whipping the head forward and back or from side to side (which often happens in motor vehicle accidents). This in turn causes the brain to collide with the bony skull in which it is enclosed, and ultimately results in bruised brain tissue and torn blood vessels. Depending on the specific mechanism of injury, damage occurs at (and in some cases opposite) the point of impact. Consequently, specific areas of the brain –usually the frontal and temporal lobes – are damaged. When this happens, MRI and CAT scans can usually detect the damage.
The rapid movement of the brain in closed head injuries can also stretch and damage neuronal axons – the long, spindly arms of nerve cells in the brain that connect cells, connect various parts of the brain, and connect the brain with the rest of the body. This widespread axonal injury interrupts regular communication within and between various brain regions and sometimes between the brain and other body parts. This type of diffuse damage usually goes undetected by available imaging technology. That being stated, its existence can be readily identified in the widespread effects it has on the individual’s ability to function.
In conclusion, after a closed head injury, damage can occur both in specific parts of the brain (due to bruising and bleeding) and throughout the brain (due to stretched or destroyed axons). The results of a closed head injury tend to have widespread effects on someone’s ability to function, primarily due to the diffuse axonal injury. The extent of damage is associated with the force of the blow to the head; for example, a head that hits a car windshield at high speed will usually sustain more tissue damage than when the vehicle is traveling at a slower speed.
Open head injury, the second type of TBI, occurs when something, such as a bullet, penetrates the skull. Damage following open head injuries tends to be concentrated, not widespread, and the implications for subsequent problems also tend to be focal and limited. However, these types of injuries can be as severe as closed head injuries, in certain circumstances.
What happens immediately after TBI?
Two effects are usually apparent in the immediate aftermath of a TBI. First, brain tissue reacts to trauma and to tissue damage through a progression of biochemical and other physiological responses. Substances that once were safely contained within the cells now flood the brain, causing additional damage and destruction of brain cells, ultimately resulting in “secondary cell death.”
The second type of effect is manifested in someone’s ability to function. For those with more severe injuries, loss of consciousness (LOC) occurs at the time of trauma, lasting from a few minutes or hours to several weeks or even months. Lengthy LOC is commonly known as coma. In such serious injuries, the first few days after trauma may also produce negative changes in respiration (breathing) and motor functions.
As an individual regains consciousness (those with the worst injuries may never do so), they may exhibit a variety of neurologically based symptoms including but not limited to irritability and aggression. Post-traumatic amnesia (PTA) is also typical when someone who is suffering from a TBI regains consciousness. PTA refers to the period when the individual experiences confusion and disorientation. Common questions at this stage are: Where am I? What happened? He or she may also have difficulty remembering or be unable to remember recent events.
With time, these responses usually subside, as the brain and other body systems are stabilized. But, unlike tissues such as bone or muscle, the neurons in the brain do not mend themselves. New nerves are not generated in a way that leads to complete recovery. In other words, certain areas of the brain remain damaged, and the person suffering from TBI may have to deal with ramifications for the rest of his or her life.
For a free legal consultation, call (212) 540-2984
How is “severity of injury” defined?
Before discussing the immediate and long-term effects of TBI in greater detail, it is important to understand how the “severity of injury” is defined.
This term is usually used to describe the extent of brain tissue damage. Although it cannot be directly measured, it is usually estimated by gauging the duration of loss of consciousness (LOC), the depth of coma and sometimes by the length of PTA.
The scale most frequently used to measure the depth of coma is the Glasgow Coma Scale (GCS). Specifically, the GCS is used to rate three aspects of functioning: eye opening, motor response, and verbal response. Individuals in deep coma score very low in all three categories, while those who aren’t as badly injured or who are recovering from coma score higher.
For example, someone with a GCS score of 3 is in the deepest level of coma and is completely unresponsive. Conversely, someone with score of 9 or more indicates that he or she is no longer in a comatose state, but is not fully alert. The highest score (15) refers to a person who is fully conscious.
The severity of brain injury is typically classified as mild (or minor), moderate and severe. In general, mild injury is one in which the patient experienced LOC for less than 20 minutes and an initial GCS of 13-15. Furthermore, an initial GCS of 9-12 defines a moderate injury and 3-8 a severe injury.
Although initial brain injury measures may predict long-term impairment in most cases, these scores do not correlate well with negative consequences in someone’s life. In fact, the initial severity of injury is only one factor that should be taken into account when considering the effects of TBI on different people.
How long does recovery take?
Recovery after injury is usually quite variable for those with moderate-to-severe injuries compared to those with mild injuries. And, as we cannot stress enough, recovery varies greatly from person to person. Thus, recovery will not be the same for any two people with TBI.
In mild TBI, one person may have a quick and full recovery, while someone else may face significant challenges even several years after they were injured.
For people with more severe injuries, recovery is a multistage process, which usually continues in a variety of ways for months and years. However, there is no standard duration for this recovery process, and the stages of recovery that are common when considering the entire population affected by TBI, may be very different for any one person. Some stages may not follow a logical progression. Instead, they may overlap, or one or more stages may be skipped altogether.
Click to contact our personal injury lawyers today
How is recovery measured right after injury?
The progress made during the immediate recovery period in individuals with severe to moderate TBI is often tracked using the Rancho Los Amigos Scale. This system includes eight levels – from the depths of coma to return to awareness and purposeful activity. These levels of recovery reflect processes within the brain, as it heals, stabilizes, and reorganizes itself to some extent.
Although the Rancho scale assumes that recovery will pass through eight stages, a small percentage of people with severe injuries remain stuck at Levels I to III for months or even years. They remain in coma or in a relatively unresponsive state and fail to return to purposeful, appropriate activity.
Rancho Los Amigos Scale
- Level I (No Response): The person is in deep coma and does not respond to any stimuli.
- Level II (Generalized Response): The person sleeps most of the time, with periods of brief wakefulness. Responses and movements are largely reflexive and not purposeful.
- Level III (Localized Response): The person is alert for longer periods. He/she reacts inconsistently to commands, but his/her responses are related to the type of stimulus presented. For example, noises will produce a listening response.
- Level IV (Confused and Agitated): As awareness increases, the person’s behavior reflects his/her sense of confusion and disorganization. He or she may engage in aggressive and/or silly behavior, along with verbal abuse, agitated actions, and incoherent speech. At this stage, his or her attention span is too short to allow full cooperation in treatment programs; and he or she is unable to do basic tasks, such as eating, independently.
- Level V (Confused, Inappropriate, Not Agitated): Simple commands are now followed consistently; the person’s long-term memory is returning; and she/he can now carry out over-learned skills such as eating. Difficulty is evident in following complex commands, short-term memory, learning new skills, and concentrating for more than a few minutes.
- Level VI (Confused, Appropriate): At this stage, someone recovering from TBI begins to show goal-directed behavior, but still needs direction in most cases. By now, he or she is more aware of his/her deficits, family members, and so forth. He/she can carry out more tasks independently and retains relearned skills from one occasion to the next.
- Level VII (Automatic, Appropriate): At this point, someone recovering from TBI is capable of performing daily routines automatically and is more adept at learning new skills, although they may not be able to do so as quickly as they could than before they were hurt. The person will still have poor short-term memory; and their judgment and problem solving are still impaired.
- Level VIII (Purposeful, Appropriate): At this stage of their recovery, the person is able to function once again in the community. However,they may still have difficulties with cognitive, social, and emotional functioning, to some extent.
Complete a Free Case Evaluation form now
Take Action and File a Brain and Spinal Cord Injury Claim Now
The financial and emotional burden of a brain injury is devastating, but our New York City spinal cord injury attorneys will make sure you receive justice for your trauma. Our legal team is dedicated to helping accident victims receive the compensation they deserve, and we are available to get to work on your case right away.
Featured Image credit: U.S. Air Force photo/Staff Sgt. Jonathon Fowler
In Post Image Credit: By GeorgeWilliams21 – Own work, CC BY-SA 4.0
Our attorneys bring years of experience to cases involving car and construction accidents, severe injuries, wrongful death, and numerous other types of personal injury.